Chapter 20
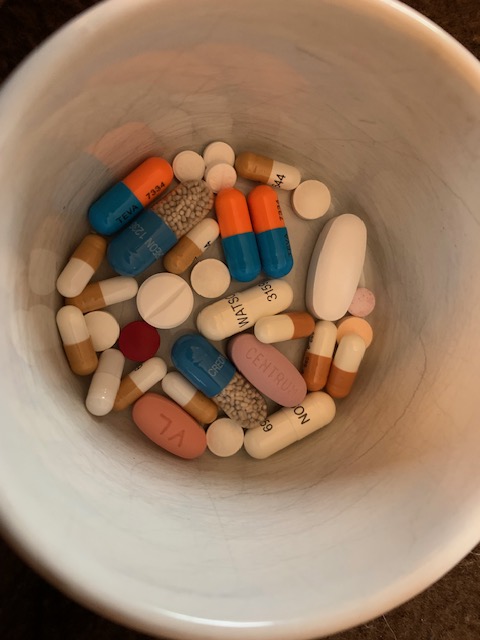
When the hospital sends you home with the piles of medication, they give you a container that looks like a zippered book. It’s a daily pill sorter with many compartments for each day, for a week’s supply. That’s not going to work if you go away for more than a week, and the doctors will tell you if you travel internationally, it’s best to take the actual pill bottles.
When I went to Sicily, I did just that. And it’s a good thing I did, because as I’ve mentioned, I ended up in the hospital for two full weeks. If I hadn’t had enough medication, the results could have been deadly. Yes, I was in a hospital, but it’s hard enough to get Envarsus here in the U.S. (this is what I take to prevent my body from rejecting the new organs). I can’t imagine what that might have been like in Sicily.
I also took all the bottles when I went to Egypt. Unlike Sicily, I wasn’t as confident of my safety in Egypt. Luckily, I was on a Viking river cruise, and they had an armed guard with us everywhere we went. But of course my active imagination conjured up all kinds of scenarios where we were kidnapped and held for ransom by some extremist group. So, I did an online search on what happens if a transplant patient doesn’t take their medication. The results are not good.
I’m naïve enough to think that since the new liver is working just fine, that not taking the immunosuppressants might not be fatal, at least not right away. That’s just not true. Here’s what I found:
*******************************************************
If a liver transplant patient doesn’t take their anti-rejection medication, several things can happen that could jeopardize their health and the success of the transplant. These medications, often called immunosuppressants, are critical because they prevent the immune system from attacking the new liver, which it may see as a foreign object. Here’s what can happen:
1. Rejection of the Transplanted Liver
The most immediate and dangerous risk is acute rejection, where the body’s immune system attacks the transplanted liver. This could lead to liver failure, which, in severe cases, can be life-threatening if not treated promptly.
- Symptoms of rejection include:
- Fever
- Jaundice (yellowing of the skin or eyes)
- Dark urine
- Abdominal pain or tenderness (especially in the upper right side)
- Fatigue or weakness
- Nausea or vomiting
2. Chronic Rejection
If the patient continues to skip medications or doesn’t follow the prescribed regimen over time, they can develop chronic rejection. This is a slower, long-term process where the liver gradually becomes damaged. It often leads to loss of liver function, and in the worst case, the need for a second transplant or even death if no intervention is made.
3. Increased Risk of Infection
Since immunosuppressants weaken the immune system, stopping the medication can increase the likelihood of infections. Without proper immune suppression, the body becomes more susceptible to viruses, bacteria, and fungi, which can complicate the recovery process and overall health.
4. Potential for Severe Complications
- Liver failure: If rejection is not controlled, it can lead to acute liver failure, which may require an urgent transplant or life-saving treatments.
- Organ Damage: The liver might suffer irreversible damage, reducing its ability to detoxify the body, produce essential proteins, and maintain blood clotting.
- Graft loss: The transplanted liver could become non-functional, and the patient might lose the new organ, making another transplant necessary.
What Should Be Done if Medication is Missed?
If a patient misses their rejection medication, it’s important to:
- Contact the transplant team: They can give guidance on what to do and might adjust medications or monitor the patient more closely.
- Follow up regularly: Regular blood tests and liver biopsies (if necessary) can help identify early signs of rejection or complications.
- Avoid missing doses in the future: Setting reminders, using a medication tracking app, or having a family member assist with the medication schedule can help prevent mistakes.
Overall Risk:
The risks of not taking rejection medications are significant, and missing even a single dose can increase the chances of the body rejecting the liver or other complications arising. For someone who has undergone a liver transplant, sticking to their medication regimen is absolutely essential for long-term success and survival.
*****************************************************
Then, I started thinking that if I pointed out to the kidnappers that I might die if they didn’t let me go, I would be released immediately and spared death. Which is laughable, because what would probably happen instead is a bullet in my head to spare them from listening to me.
But it’s good for me to know the consequences (I don’t have any plans to stop taking my pills, I just like to know these things).
Then, because I am nothing if not thorough, and I’ve already been told by the doctors that people with a new liver go back to drinking, I wanted to know how quickly that would explode. Here’s what I found:
************************************************************
If a liver transplant patient starts drinking alcohol again, it can have serious and potentially life-threatening consequences. Even if the patient has a healthy liver after the transplant, drinking alcohol can jeopardize both the transplanted liver and their overall health. Here’s why:
1. Risk of Rejection
Alcohol can interfere with the immunosuppressive medications that transplant patients need to take to prevent organ rejection. Alcohol can make the liver less effective at metabolizing the drugs, or it may interact with them in unpredictable ways, increasing the risk of acute rejection of the new liver.
2. Damage to the Transplanted Liver
The liver is responsible for processing alcohol in the body. Even a small amount of alcohol can be toxic to the liver. For someone who has had a liver transplant, the new liver is often more vulnerable to damage from alcohol since it may not have the same resilience as a healthy, native liver.
- Alcohol can cause cirrhosis: Regular drinking can lead to fibrosis or cirrhosis of the transplanted liver, which can impair liver function and lead to failure.
- Inflammation: Alcohol can cause inflammation of the liver, which can trigger rejection episodes or other complications.
3. Increased Risk of Complications
- Infections: Immunosuppressants already put the body at higher risk for infections, and alcohol can further impair the immune system, making the patient more susceptible to illnesses.
- Gastrointestinal bleeding: Alcohol increases the risk of bleeding in the gastrointestinal tract, which can be especially dangerous if the patient has already undergone a major surgery like a liver transplant.
4. Alcohol’s Effect on Medications
Many liver transplant patients are on a complex regimen of medications to prevent rejection, manage their condition, and address other health issues. Alcohol can interfere with these medications, especially immunosuppressive drugs like tacrolimus, cyclosporine, or mycophenolate, either by reducing their effectiveness or increasing side effects. This interaction could lead to:
- Toxicity: The buildup of medications in the bloodstream can cause toxic side effects.
- Reduced effectiveness: Alcohol can make these medications less effective, which can increase the chances of organ rejection or other complications.
5. Mental and Physical Health Concerns
- Addiction: After a transplant, some patients may feel emotionally vulnerable and use alcohol as a way to cope with stress, depression, or anxiety. Drinking heavily or regularly can lead to alcohol dependence.
- Increased risk of liver failure: Drinking alcohol can put extra strain on the liver, even a transplanted one, which could accelerate the progression toward liver failure or other chronic liver diseases.
6. Impact on Overall Recovery
Alcohol can affect a patient’s ability to heal and recover from surgery. It can impair wound healing, disrupt sleep, and increase the risk of complications, all of which can delay the recovery process after a liver transplant.
Medical Advice:
- No safe amount of alcohol: Most liver transplant centers will advise complete abstinence from alcohol. While moderate drinking might be acceptable for some people with chronic liver disease (but not transplant recipients), for someone who has had a liver transplant, even small amounts of alcohol can be harmful.
- Work with the healthcare team: If a liver transplant patient is struggling with alcohol use, it’s essential to talk to their transplant team, counselors, or addiction specialists. They can provide resources and strategies for managing the urge to drink and help avoid alcohol-related complications.
Key Takeaways:
- Alcohol can cause rejection and may interact with immunosuppressant medications, increasing the risk of transplant failure.
- Drinking alcohol can lead to liver damage, cirrhosis, and even failure of the transplanted liver.
- Abstinence from alcohol is usually recommended to protect the new liver and maintain good health.
It’s essential for liver transplant patients to follow the advice of their transplant team closely, and that often includes staying away from alcohol entirely. If you or someone you know is in this situation, it’s important to have open discussions with healthcare providers about any concerns or challenges related to alcohol use.
**************************************************
Remember the survey I took at my liver doctor’s office? The one where the nurse told me it’s surprisingly common to find transplant patients drinking again? I want to send them all this information. While it’s tempting to think “oh, I’ll just have one drink, that won’t hurt anything,” and maybe it won’t, but what are the chances you’ll stop at one? Virtually none. That’s why I CAN’T ever drink again. And I know this, and I won’t. For me, it’s very easy to abstain when I know it will kill me. Talk about motivation.
So there you have it. Now you’re a transplant expert!






Leave a comment